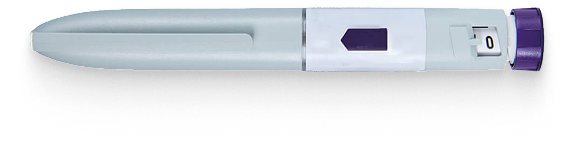
Dehydration is a potential complication that can occur in people using GLP-1 receptor agonist injections, such as semaglutide (Wegovy) and tirzepatide (Mounjaro), for weight management or diabetes control. It develops when the body loses more fluids than it takes in, disrupting the normal balance of electrolytes.
With GLP-1 injections, dehydration isn’t usually a direct side effect. Instead, it typically develops because of other side effects these medications can cause, including: nausea, vomiting, and diarrhoea, or due to reduced fluid intake when experiencing symptoms like dry mouth.
For instance, if you’re feeling sick, been sick, or having diarrhoea, your body is losing fluids rapidly. Similarly, some people experience dry mouth and simply don’t drink enough water while on these medications.
This isn’t just a minor concern. In the UK, the Medicines and Healthcare products Regulatory Agency (MHRA) has issued warnings about severe dehydration in people taking these injections. Some cases have been severe enough to require hospital treatment.
This highlights why proper monitoring and support are essential when you’re taking these powerful medications.
Key symptoms
- Increased thirst and dry mouth
- Dark-coloured urine or decreased urination
- Fatigue or weakness
- Dizziness or lightheadedness, especially when standing
- Headache
- Dry skin that lacks elasticity
- Sunken eyes
- Rapid heartbeat
- Confusion or irritability (in more severe cases)
How common is dehydration with GLP-1 treatments?
While dehydration itself is not typically reported as a direct side effect in clinical trials, the risk stems from the common gastrointestinal side effects that can lead to fluid loss. Patients may experience dehydration or related complications during GLP-1 therapy. Risk is highest during the initial titration phase and subsequent dose increases, particularly in vulnerable populations such as older adults or those with pre-existing conditions.
Managing hydration on GLP-1 treatments
Preventative strategies
- Increase fluid intake to at least 2-3 litres daily (unless contraindicated)
- Monitor urine colour – aim for pale yellow as an indicator of good hydration
- Establish a regular drinking schedule rather than relying on thirst
- Use oral rehydration solutions if experiencing significant fluid losses
- Track daily fluid intake using a dedicated water bottle or app
Dietary considerations
- Consume hydrating foods (fruits, vegetables, soups, broths)
- Replace electrolytes lost through vomiting or diarrhoea
- Limit caffeine and alcohol which can worsen dehydration
- Consider small, frequent sips if nausea makes drinking difficult
- Include foods with high water content like cucumber, watermelon, and celery
Monitoring approaches
- Weigh yourself regularly – rapid weight loss may indicate fluid loss
- Check for skin turgor by pinching skin on the back of hand. If skin doesn’t snap back quickly it can be an indicator of low hydration.
- Be alert to dizziness when changing positions
- Monitor blood pressure if possible, as dehydration can cause drops
- Note frequency and colour of urination throughout the day
Medical considerations
- Adjust medication timing to minimise side effects that contribute to dehydration
- Consider temporary dose adjustment in consultation with your healthcare provider
- Discuss anti-nausea or anti-diarrhoeal medications if these symptoms are contributing to fluid loss
- Consider IV fluids for severe cases (requires medical intervention)
When to seek medical advice
Contact your healthcare provider immediately if you experience:
- Severe thirst that cannot be satisfied by drinking
- Little or no urination for 8 hours or more
- Dizziness or lightheadedness that impairs functioning
- Confusion, disorientation, or extreme fatigue
- Rapid heart rate or breathing
- Fainting or severe weakness
- Inability to keep fluids down due to vomiting
Long-term outlook
With proper management, most patients can maintain adequate hydration whilst on GLP-1 treatments. Dehydration risk typically decreases after a few weeks as gastrointestinal side effects subside for the majority of patients.
FAQs
Does dehydration affect how well GLP-1 medications work?
Whilst moderate dehydration doesn’t directly impact the effectiveness of the medication, severe dehydration could potentially affect overall metabolism and medication absorption.
Are some people at higher risk for dehydration on GLP-1 treatments?
Yes, older adults, those taking diuretic medications, people with kidney disease, and individuals with physically demanding jobs or who exercise intensely may have increased risk.
Should I temporarily stop my medication if I become dehydrated?
Never discontinue medication without consulting your healthcare provider. However, if you’re experiencing signs of dehydration, contact them promptly for guidance.
How can I tell if my symptoms are from dehydration or from the medication itself?
Dehydration symptoms typically worsen throughout the day if fluids aren’t replenished, whilst medication side effects often follow a pattern related to injection timing. Your healthcare provider can help determine the cause.
Can drinking too much water be harmful while on GLP-1 medications?
While proper hydration is important, excessive water intake (more than 3-4 litres daily) without electrolyte replacement could potentially cause electrolyte imbalances. Focus on consistent, adequate hydration rather than extreme water consumption.