Withdrawal from GLP-1 injections requires careful planning and medical supervision to manage the return of appetite, potential weight regain, and other physiological changes. Whether you’re stopping Semaglutide (Ozempic, Wegovy), Tirzepatide (Mounjaro), or another GLP-1 medication due to side effects, cost, or personal choice, understanding how to discontinue safely can help you protect the progress you’ve worked so hard for.
It’s important to remember that obesity is a chronic, relapsing condition, much like high blood pressure or diabetes. For many people, long-term management may involve staying on the lowest effective dose of medication alongside healthy lifestyle changes. This isn’t a matter of willpower — it’s biology. Recognising this helps set realistic expectations if you do decide to withdraw.
While most GLP-1 injections can be stopped abruptly from a safety perspective, the effects on appetite, blood sugar, and weight may return gradually. Having a plan in place can help you manage these changes and protect the progress you’ve worked so hard for.
What Happens When You Stop GLP-1s?
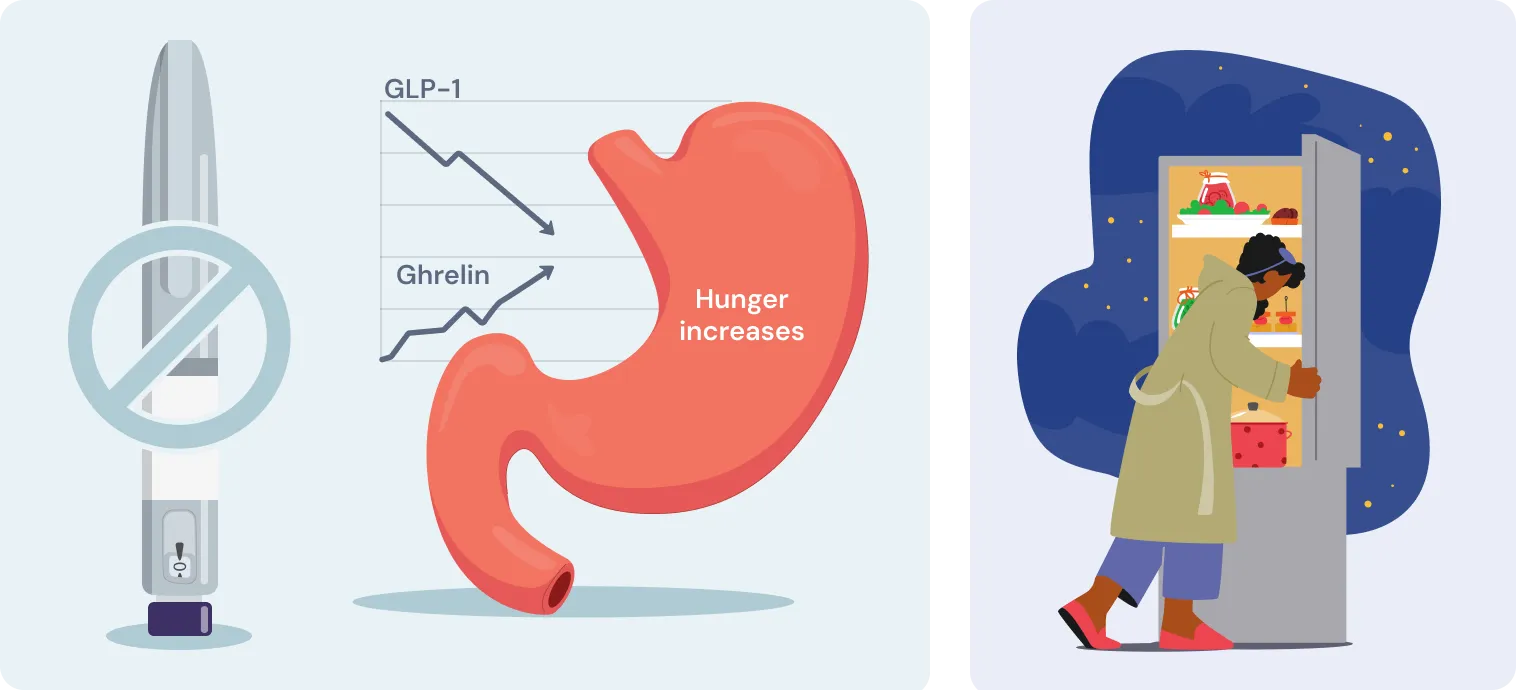
GLP-1s work by mimicking natural hormones that regulate hunger, slow digestion, and help control blood sugar. Once you stop, those effects fade and your body gradually resets.
Timeline of Changes After Stopping
Week 1–2:
- Hunger and cravings begin to return
- You may notice food on your mind more often
- Energy levels may dip slightly
Week 2–4:
- Digestion speeds up again
- Blood sugar may rise, especially if you have diabetes
- Some weight regain may begin
Month 1–3:
- Appetite returns to pre-treatment levels
- Greater risk of significant weight regain
- Blood sugar and metabolism return to baseline
Common Withdrawal Experiences & Symptoms
Physical changes:
- Increased hunger and food cravings
- Feeling hungrier sooner after meals
- Blood sugar fluctuations (important for those with diabetes)
- Possible nausea as eating patterns shift
Emotional and mental changes:
- Worry or anxiety about weight regain
- Feeling disappointed if stopping wasn’t your choice
- Relief from side effects, but new concerns about what comes next
Why Medical Support Matters
Your body doesn’t flip a switch when you stop GLP-1s. Appetite, blood sugar, digestion, and mood can all shift in ways that aren’t always predictable.
Think of it like blood pressure: people often need ongoing medication even after their readings improve. Weight is similar. It’s a long-term condition, and relapse is common if it’s not actively managed.
Working with a clinician means:
- Any changes are spotted early
- Risks like sudden blood sugar spikes or rapid regain are reduced
- You have guidance on whether to stay off, restart, or adjust your dose
In short, medical support gives you a safety net so you’re not left guessing.
How to Support Your Body During Withdrawal
🍽 Nutrition & Appetite Management
- Keep healthy, filling foods in the house
- Plan meals in advance
- Eat slowly, using smaller plates
- Stop eating when you’re about 80% full
- Pause 20 minutes before going for seconds
- Stay hydrated and identify emotional vs physical cravings
💉 Blood Sugar Management (for those with diabetes)
- Check levels more frequently during the first month
- Stick to a regular eating routine
- Balance carbs with protein and healthy fats
- Be ready to adjust your other diabetes medications
⚖️ Weight Management Tips
- Know that some weight regain is normal
- Focus on sustainable habits, not just the number on the scale
- Celebrate non-scale victories: energy, sleep, strength
- Keep moving: aim for at least 150 minutes of activity a week
🧠 Mental Health & Support
- Be kind to yourself—this is a transition
- Talk to a counsellor or join a support group if needed
- Use healthy coping strategies for stress
- Focus on overall health, not just weight
Alternative Options and Next Steps
Other Weight Management Medications (UK-Approved)
- Orlistat (available as Alli over the counter) Works by reducing fat absorption in the gut. Best used alongside a low-fat diet.
- Liraglutide (Saxenda) A daily injectable GLP-1 medication licensed for weight management. Often prescribed through specialist weight management services.
- Setmelanotide Only approved for use in very rare genetic conditions like POMC (pro-opiomelanocortin) deficiency and under strict specialist supervision.
Non-Medication Approaches (NHS and Private Options)
- NHS Digital Weight Management Programme Free for eligible patients with high BMI and diabetes/hypertension. Includes coaching and structured guidance.
- Referral to Tier 3 or Tier 4 Weight Management Services Includes support from a multidisciplinary team—dietitians, psychologists, physicians—for patients meeting specific criteria.
- Structured Meal Replacement Plans Programmes like Counterweight-Plus (used in the DiRECT trial) may be offered through specialist NHS services or privately.
- Behavioural Therapy Programmes Includes CBT-based support for emotional eating, body image, and long-term weight regulation. May be offered via NHS or private clinics.
- Bariatric Surgery Consultation Available on the NHS for qualifying patients, often through Tier 4 services. Includes options like gastric bypass, sleeve gastrectomy, or banding.
Returning to GLP-1 Therapy
- Treatment breaks can be temporary; restarting may be possible if your circumstances or health needs change.
- Supply or availability issues may resolve over time.
- Side effects might improve with a lower starting dose or different GLP-1 formulation.
- Alternative GLP-1 medications (e.g. Saxenda, Wegovy, Mounjaro) may be better tolerated—though NHS access varies depending on your region and clinical need.
Looking Ahead: A Promising Future
The landscape of weight management is evolving rapidly. New and improved weight loss therapies are on the horizon, including next-generation GLP-1s, combination treatments, and novel approaches in development. They are calling it the Metabolic Health Revolution.
It’s an exciting and hopeful time for anyone looking to manage their weight more effectively, with more personalised options becoming available every year.
Your GP or pharmacists can help you stay informed and choose the right treatment path for your needs, whether that’s now or in the future.
When to Seek Immediate Medical Attention
Please contact your healthcare provider right away if you notice:
- Severe blood sugar spikes or symptoms of diabetic ketoacidosis (e.g. nausea, fruity breath, confusion)
- Uncontrolled binge eating
- Severe anxiety, low mood, or thoughts of self-harm
- Rapid weight gain with no explanation
Your Personal Withdrawal Plan: A Checklist
Before Stopping:
- Discuss timeline with healthcare provider
- Schedule regular follow-up appointments
- Plan blood sugar monitoring schedule (if diabetic)
- Prepare meal plans and grocery lists
- Identify support systems and resources
- Set realistic expectations and goals
- Consider alternative treatment options
During Withdrawal:
- Daily weight tracking (optional, based on personal preference)
- Blood sugar logs (if diabetic)
- Appetite and hunger level tracking
- Mood and energy level notes
- Physical activity records
- Medication adherence for other conditions
For Long-Term Success:
- Regular healthcare provider check-ins
- Sustainable eating pattern establishment
- Consistent exercise routine
- Stress management practices
- Support group participation
- Realistic goal reassessment
Summary
Withdrawal from GLP-1 injections is safe when guided by a healthcare professional. Success depends on preparing for the return of appetite, keeping healthy habits, and setting realistic expectations about possible weight regain.
Remember: weight regulation is a chronic, relapsing condition, just like high blood pressure or diabetes. Stopping medication doesn’t mean failure — it means you and your clinician are adjusting your approach. For many, the best long-term strategy is combining lifestyle changes with the lowest effective dose of treatment.
Your health journey is unique. Focus on sustainable habits, stay connected with your care team, and know that managing weight is a long-term process with many possible strategies along the way.
Frequently Asked Questions
Can I stop GLP-1 injections suddenly?
Yes — from a medical safety point of view, you usually can. But planning ahead helps manage appetite and weight changes, so it’s always best to do so under supervision.
How quickly will my hunger return?
Most people notice a change within 1–2 weeks. Full appetite usually returns within a month, as the medication’s effects fade and your body resets.
Will I regain the weight?
Some regain is common, because weight is a chronic and relapsing condition. Studies suggest 50–80% of lost weight may return without ongoing support. This isn’t about willpower — it’s about biology. That’s why continuing healthy habits, or sometimes staying on the lowest effective dose of medication, makes long-term success more likely.
Can I go back on GLP-1s later?
Absolutely. Many people restart, especially if they stopped due to cost, supply issues, or short-term side effects. Sometimes a lower dose or a different GLP-1 works better the second time around.
What should I expect if I have diabetes?
Your blood sugar may gradually rise again as appetite and digestion return to baseline. You’ll likely need to monitor more frequently and adjust other medications with your healthcare provider’s guidance.