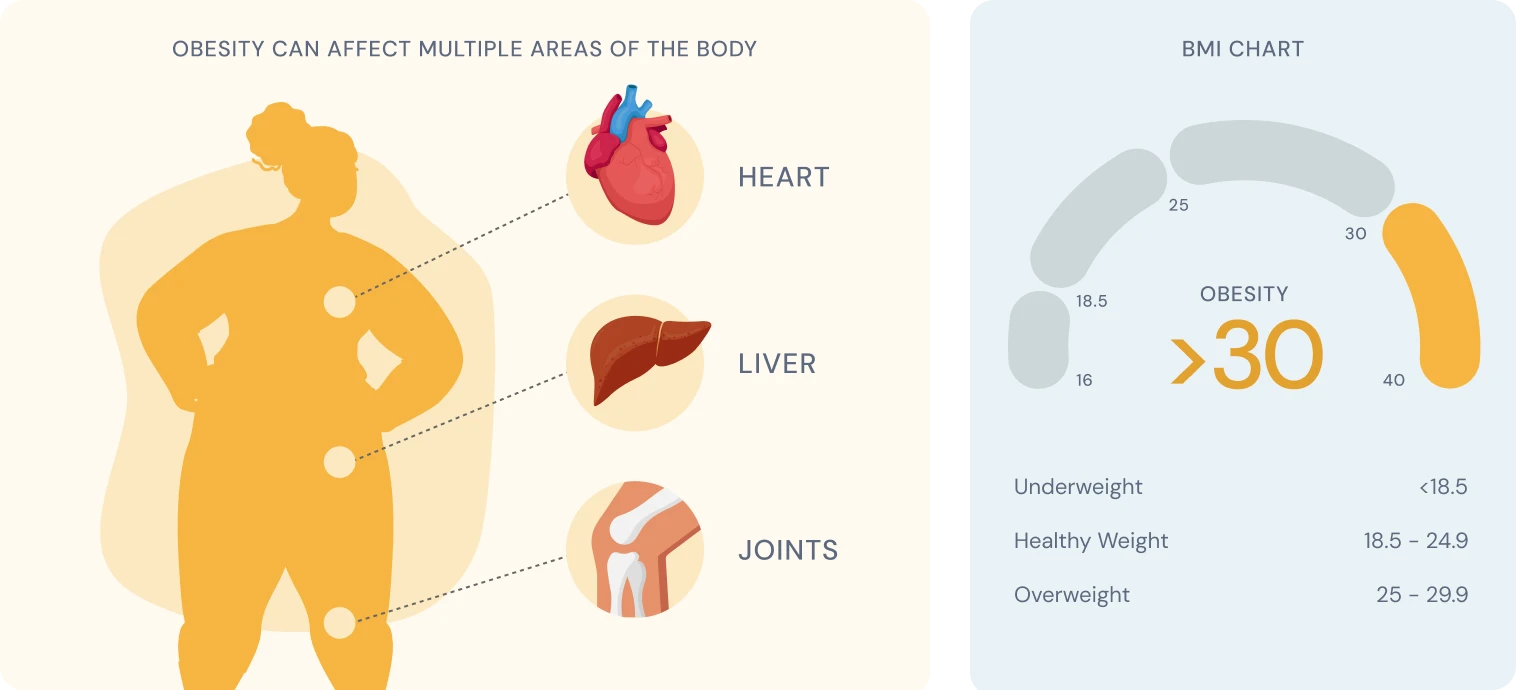
Obesity is a complex medical condition characterised by excess body fat accumulation to the extent that it may impair health.
Doctors typically diagnose obesity when your Body Mass Index (BMI) reaches 30 kg/m² or higher. However, BMI is just one tool and doesn’t tell the whole story. It doesn’t consider important factors like how much muscle you have or where your body stores fat.
Medical understanding of obesity has evolved significantly. Today, healthcare professionals recognise it as a chronic disease requiring ongoing management – similar to conditions like diabetes or high blood pressure – rather than simply a lifestyle choice or lack of willpower.
This shift in perspective has important implications for treatment approaches and how we support those living with obesity.
Key characteristics
- BMI of 30 kg/m² or above (for adults)
- Excess body fat, particularly around the abdomen
- Often associated with various health complications
- Can significantly impact quality of life
- Frequently requires multi-faceted treatment approaches
- Considered a chronic condition requiring ongoing management
How common is obesity?
Obesity has reached epidemic proportions in the UK, affecting approximately 28% of adults. The prevalence has nearly tripled since 1980, and current trends suggest continued increases. Childhood obesity has also risen dramatically, with about 15% of 2-15 year olds living with obesity. These statistics highlight obesity as one of the most significant public health challenges facing the UK today.
Understanding obesity
Causes and risk factors
- Genetic factors: Research indicates that genetics may account for 40-70% of obesity susceptibility
- Environmental influences: Food availability, portion sizes, food marketing, and urban design that discourages physical activity
- Psychological factors: Emotional eating, stress, depression, and anxiety can influence eating behaviours
- Medical conditions: Hypothyroidism, Cushing’s syndrome, polycystic ovary syndrome (POS), and certain medications can contribute to weight gain
- Sleep deprivation: Poor sleep quality or duration can disrupt hormones that regulate hunger and appetite
- Gut microbiome: Emerging research suggests gut bacteria composition may play a role in obesity
Health implications
Obesity significantly increases the risk of numerous health conditions, including:
- Type 2 diabetes mellitus
- Cardiovascular disease (heart disease, stroke, hypertension)
- Certain cancers (including breast, colorectal, and endometrial)
- Osteoarthritis
- Sleep apnoea and respiratory problems
- Mental health conditions (depression, anxiety)
- Non-alcoholic fatty liver disease
- Reduced life expectancy (by an average of 3-10 years)
Managing obesity
Lifestyle interventions
- Dietary changes: Focus on balanced nutrition with appropriate calorie intake; evidence from systematic reviews suggests that the specific diet (Mediterranean, low-carb, etc.) matters less than finding a sustainable approach
- Hydration: Staying well-hydrated is a simple yet powerful lifestyle change that supports weight management by curbing appetite, boosting metabolism and improving overall health
- Physical activity: Aim for at least 150 minutes of moderate activity weekly, with additional resistance training; particularly beneficial for maintaining weight loss
- Behavioural therapy: Cognitive behavioural techniques to address eating triggers, develop coping strategies, and modify unhealthy habits
- Sleep optimisation: Improving sleep quality and duration can positively impact weight management
- Stress management: Techniques such as mindfulness, meditation, and yoga to reduce stress-related eating
Medical approaches
- Anti-obesity medications: Several medications that are also available on NHS prescription including:
- Bariatric surgery: Procedures such as gastric band, sleeve gastrectomy, or gastric bypass for those with severe obesity or obesity with complications
- Specialist weight management services: Multi-disciplinary teams providing comprehensive support
- Emerging treatments: New medications and approaches continue to be developed and approved
Over-the-counter pharmacy aids in the UK
- Orlistat (Alli): Lower-dose version of prescription Xenical, available without prescription
- Meal replacements: Products like meal replacement shakes and bars
- Caffeine supplements: Claimed to increase metabolism, though effects are modest
- Chromium supplements: Marketed for blood sugar regulation and reducing cravings
It’s important to note that OTC products should be used alongside, not instead of, healthy eating and physical activity.
When to seek medical advice
Contact your healthcare provider if:
- Your BMI is 30 kg/m² or above (or 27 kg/m² with weight-related health problems)
- You’ve struggled to lose weight despite significant efforts with diet and exercise
- You have symptoms of weight-related health problems (joint pain, difficulty breathing, excessive fatigue)
- You experience sudden or unexplained weight gain
- You’re concerned about your child’s weight
- You’re considering weight loss surgery or prescription medications
Long-term outlook
Obesity is best understood as a chronic condition requiring ongoing management rather than a problem to be “cured.” Successful long-term weight management typically involves:
- Sustainable lifestyle changes rather than short-term “diets”
- Ongoing support systems (professional and/or personal)
- Regular monitoring and adjustment of strategies
- Addressing psychological aspects of eating and weight
- Acceptance that some weight fluctuation is normal and expected
Most people can achieve clinically significant health benefits with modest weight loss of 5-10% of initial body weight, even if they remain in the “overweight” or “obese” BMI category.
FAQs
Is obesity simply the result of eating too much and exercising too little?
No, obesity is far more complex than this oversimplification suggests. While energy balance (calories in vs calories out) is important, numerous factors influence this balance including genetics, hormones, gut microbiome, medication, psychological factors, and environmental influences. This is why simple advice to “eat less, move more” is often ineffective on its own.
Can some people be “healthy at any size”?
The relationship between weight and health is complex. Some people with obesity may not have immediate health problems (sometimes called “metabolically healthy obesity“), but research shows this state is often temporary. However, health improvements can occur independently of weight loss through better nutrition and increased physical activity.
Why do most diets fail in the long term?
Most traditional diets fail because they:
- Are too restrictive and unsustainable
- Trigger biological adaptations that increase hunger and reduce metabolism
- Don’t address psychological and environmental factors
- End after a specific timeframe rather than transitioning to maintenance strategies
- Fail to account for individual differences in response to dietary approaches
Should I try to lose weight quickly or slowly?
Research indicates that moderate, sustainable weight loss of 0.5-1 kg per week is associated with better long-term outcomes than rapid weight loss. However, some structured programmes with very low calorie diets under medical supervision may have a role for specific individuals.
Can medications alone solve obesity? While newer medications like GLP-1 receptor agonists show promising results, they work best when combined with lifestyle changes. Additionally, weight regain is common if medication is discontinued, highlighting the importance of comprehensive approaches to treatment.
Related
- Bloating from GLP-1 Injections
- Common GLP-1 Weight-loss Side Effects
- Constipation from GLP-1 Injections
- Dehydration from GLP-1 Injections
- Diarrhoea from GLP-1 Injections
- Dry Mouth from GLP-1 Injections
- Injectable Weight Loss Treatments (GLP-1)
- Nausea & Vomiting from GLP-1 Injections
- Sulphur Burps from GLP-1 Injections (Mounjaro, Wegovy): How to Manage Them
- Diarrhoea
- Weight Loss